Can Antibiotics Constipate You

Have you ever experienced constipation after taking antibiotics? It's a common concern that many individuals face. In this blog post, we will delve into the relationship between antibiotics and constipation, exploring the causes, symptoms, and potential solutions. Understanding how antibiotics can impact your digestive system is crucial for maintaining overall well-being.
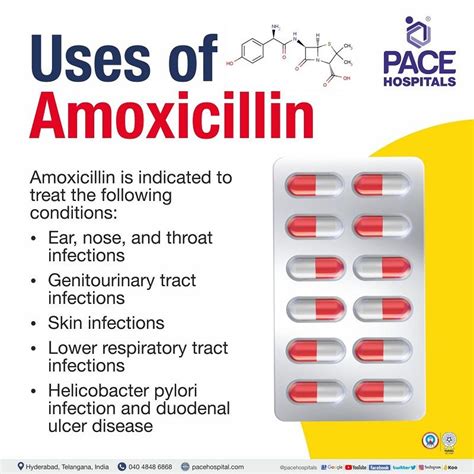
Understanding Antibiotics and Their Impact on the Body

Antibiotics are powerful medications designed to fight bacterial infections. They work by either killing the bacteria or inhibiting their growth, allowing the body's immune system to overcome the infection. While antibiotics are effective in treating various illnesses, they can also have unintended side effects, including constipation.
Constipation is a common digestive issue characterized by infrequent bowel movements, hard stools, and difficulty passing them. It can cause discomfort, bloating, and a general feeling of unease. When antibiotics are prescribed, it's essential to be aware of their potential impact on bowel movements and take necessary precautions.
How Antibiotics Lead to Constipation

Antibiotics can disrupt the delicate balance of bacteria in the gut, known as the gut microbiome. This disruption can have a ripple effect on the digestive system, leading to constipation. Here's how it happens:
- Altered Gut Microbiome: Antibiotics are not selective in their action. They target both harmful and beneficial bacteria in the gut. By reducing the population of good bacteria, antibiotics can disrupt the normal functioning of the digestive system.
- Reduced Water Absorption: The gut microbiome plays a crucial role in maintaining the water balance in the colon. When the balance is disrupted, the colon may absorb excess water from the stool, making it harder and more difficult to pass.
- Impaired Muscle Contractions: The gut relies on muscle contractions to move food and waste through the digestive tract. Antibiotics can interfere with these contractions, leading to slower transit time and constipation.
Recognizing the Symptoms of Antibiotic-Induced Constipation

Identifying the symptoms of antibiotic-induced constipation is essential for timely management. Here are some common signs to look out for:
- Infrequent Bowel Movements: A noticeable decrease in the frequency of bowel movements is a red flag. Normally, individuals should have at least three bowel movements per week.
- Hard and Dry Stools: Constipation often results in the production of hard, dry stools that are difficult to pass. This can cause discomfort and pain during bowel movements.
- Abdominal Discomfort: Individuals may experience bloating, cramping, and a feeling of fullness in the abdomen due to the buildup of waste in the intestines.
- Straining During Bowel Movements: Constipation can make it challenging to pass stools, leading to excessive straining and potential injury to the rectal muscles.
Managing Antibiotic-Induced Constipation

If you find yourself constipated while taking antibiotics, there are several strategies you can employ to alleviate the discomfort and promote regular bowel movements.
Increase Fluid Intake

Drinking plenty of fluids, especially water, is crucial for preventing and managing constipation. Adequate hydration helps soften the stool, making it easier to pass. Aim for at least 8-10 glasses of water per day.
Eat Fiber-Rich Foods

Incorporating fiber-rich foods into your diet can work wonders for constipation. Fiber adds bulk to the stool, promoting regular bowel movements. Include fruits, vegetables, whole grains, and legumes in your meals to boost your fiber intake.
Exercise Regularly

Physical activity plays a vital role in maintaining a healthy digestive system. Regular exercise, such as walking, jogging, or yoga, can stimulate bowel movements and improve overall gut motility.
Consider Over-the-Counter Remedies
If constipation persists, over-the-counter laxatives or stool softeners can provide temporary relief. However, it's essential to consult with a healthcare professional before using any medication, especially if you are already taking antibiotics.
Stay Active and Maintain a Healthy Lifestyle

Maintaining a healthy lifestyle is key to preventing and managing constipation. Ensure you get enough rest, manage stress levels, and avoid excessive alcohol consumption. A balanced diet and regular exercise routine will go a long way in keeping your digestive system functioning optimally.
Prevention is Key

While managing constipation is important, preventing it from occurring in the first place is even better. Here are some tips to reduce the risk of antibiotic-induced constipation:
- Discuss with your healthcare provider: Before starting antibiotics, consult with your doctor or pharmacist about potential side effects and ways to prevent them.
- Probiotics: Consider taking probiotic supplements or consuming probiotic-rich foods like yogurt. Probiotics can help restore the balance of good bacteria in the gut.
- Stay Hydrated: Make sure to drink plenty of fluids throughout the day, especially when taking antibiotics.
- Fiber Intake: Ensure you are getting an adequate amount of fiber in your diet to promote regular bowel movements.
When to Seek Medical Attention

While constipation is generally not a cause for immediate concern, there are situations where medical attention is necessary. If you experience any of the following symptoms, it's important to consult with a healthcare professional:
- Severe abdominal pain or cramping.
- Blood in the stool or on the toilet paper.
- Prolonged constipation lasting more than a week.
- Unexplained weight loss.
- Nausea, vomiting, or fever accompanying constipation.
Remember, it's always best to seek professional advice when dealing with any health concerns.
Conclusion

Antibiotics are essential medications for fighting bacterial infections, but they can sometimes lead to constipation. By understanding the causes and symptoms of antibiotic-induced constipation, you can take proactive measures to manage and prevent it. Remember to stay hydrated, incorporate fiber-rich foods into your diet, and maintain a healthy lifestyle. If constipation persists or worsens, don't hesitate to reach out to a healthcare professional for guidance.
Can all antibiotics cause constipation?

+
While constipation is a common side effect of antibiotics, not all antibiotics have the same impact. Certain types of antibiotics are more likely to cause constipation due to their specific mechanisms of action. It’s important to discuss any concerns with your healthcare provider.
How long does antibiotic-induced constipation typically last?

+
The duration of antibiotic-induced constipation can vary. In most cases, it resolves within a few days to a week after completing the antibiotic course. However, it’s important to monitor your symptoms and seek medical advice if constipation persists.
Are there any natural remedies to relieve antibiotic-induced constipation?

+
Yes, there are several natural remedies that can help alleviate constipation. These include increasing fluid intake, consuming prunes or prune juice, and trying herbal teas like senna or peppermint. However, it’s important to consult with a healthcare professional before trying any new remedies.
Can antibiotic-induced constipation lead to more serious health issues?

+
In most cases, antibiotic-induced constipation is a temporary and manageable issue. However, if left untreated or if severe, it can lead to complications such as hemorrhoids, anal fissures, or even bowel obstruction. It’s crucial to address constipation promptly to prevent further health problems.
Is it safe to take laxatives while on antibiotics?

+
It is generally safe to take over-the-counter laxatives while on antibiotics, but it’s important to consult with a healthcare professional first. They can guide you on the appropriate type and dosage of laxative to use. Self-medicating without professional advice should be avoided.