The Ultimate 10Step Guide To Handling Cephalopelvic Disproportion Today
Understanding Cephalopelvic Disproportion (CPD): A Comprehensive Guide

When it comes to childbirth, one of the most concerning situations for expectant mothers and healthcare professionals is Cephalopelvic Disproportion (CPD). CPD occurs when the baby's head is too large to fit through the mother's pelvis, leading to potential complications during labor and delivery. In this ultimate 10-step guide, we will explore the ins and outs of CPD, offering valuable insights and practical advice for managing this challenging condition.
Step 1: Recognizing the Signs of CPD
Early detection is crucial in managing CPD effectively. Here are some key signs and symptoms that may indicate the presence of CPD:
- A history of difficult or prolonged labor in previous pregnancies
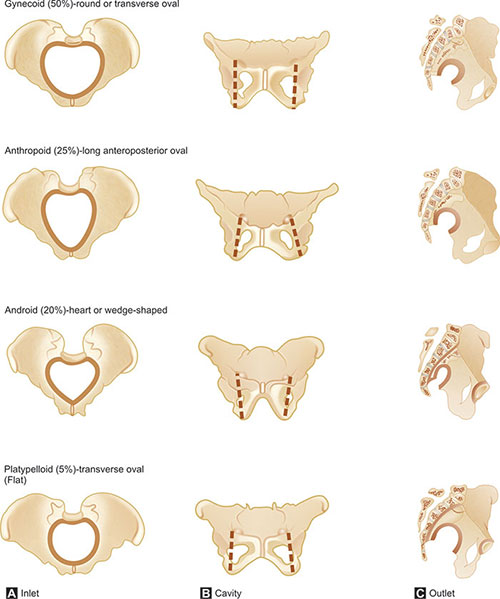
- Small or abnormally shaped pelvis
- Large baby, often estimated through ultrasound measurements
- Pelvic pain or discomfort during pregnancy
- Slow or stalled labor progress
If you or your healthcare provider suspect CPD, further evaluation is necessary to confirm the diagnosis and develop an appropriate management plan.
Step 2: Diagnostic Procedures for CPD

Several diagnostic procedures can help confirm CPD and assess the severity of the condition. These may include:
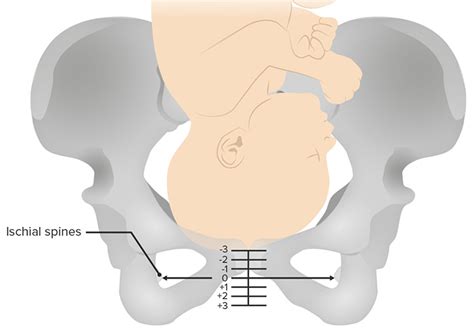
- Pelvimetry: A physical examination of the pelvis to assess its size and shape. This can be done externally or internally.
- Ultrasound: An ultrasound can provide accurate measurements of the baby's head and body, helping to determine if CPD is present.
- X-rays: In some cases, X-rays may be used to evaluate the pelvic bones and their relationship to the baby's head.
- Magnetic Resonance Imaging (MRI): An MRI can provide detailed images of the pelvis and baby's position, offering valuable information for decision-making.
The choice of diagnostic procedure depends on various factors, including the stage of pregnancy, the suspected severity of CPD, and the availability of resources.
Step 3: Understanding the Causes of CPD

CPD can occur due to a variety of factors, including:
- Maternal Factors: Certain maternal characteristics, such as a small or abnormally shaped pelvis, can contribute to CPD. Previous pregnancies with CPD or a history of pelvic trauma may also increase the risk.
- Fetal Factors: A large baby, often referred to as macrosomia, is a common cause of CPD. This can be due to genetic factors, maternal diabetes, or other conditions that lead to excessive fetal growth.
- Positioning: The baby's position in the uterus can also impact the likelihood of CPD. Certain positions, such as a transverse lie or a persistent occiput posterior position, may make it more challenging for the baby to navigate through the birth canal.
Understanding the underlying causes of CPD is essential for developing an effective management plan and minimizing the risk of complications.
Step 4: Managing CPD During Pregnancy

Once CPD is diagnosed, the focus shifts to managing the condition during pregnancy to ensure the best possible outcome for both mother and baby. Here are some key strategies:
- Regular Prenatal Care: Attend all scheduled prenatal appointments to monitor the progress of your pregnancy and the growth of your baby. Your healthcare provider can provide personalized advice and guidance based on your specific situation.
- Ultrasound Monitoring: Regular ultrasound scans can help track the baby's growth and position, allowing your healthcare team to make informed decisions about the timing and mode of delivery.
- Pelvic Floor Exercises: Strengthening the pelvic floor muscles through exercises like Kegels can help prepare the pelvis for childbirth and potentially reduce the risk of CPD-related complications.
- Diet and Lifestyle Modifications: A healthy diet and regular exercise, as recommended by your healthcare provider, can support optimal fetal growth and overall well-being.
Working closely with your healthcare team and following their advice is crucial for managing CPD effectively during pregnancy.
Step 5: Preparing for Delivery with CPD

As the due date approaches, it's essential to prepare for delivery with CPD. Here's what you can expect:
- Discuss Delivery Options: Collaborate with your healthcare provider to discuss the best mode of delivery for your specific situation. This may include a planned cesarean section (C-section) or attempting a vaginal delivery with close monitoring and support.
- Plan for a C-Section: If a C-section is recommended, understand the procedure, the potential risks and benefits, and the recovery process. Ask questions and address any concerns you may have.
- Vaginal Delivery with CPD: In some cases, a vaginal delivery may be attempted with CPD. This decision will be based on various factors, including the baby's position, the size of the pelvis, and the progress of labor. Close monitoring and support from a skilled healthcare team are essential.
Remember, the goal is to ensure a safe and healthy delivery for both you and your baby, and your healthcare team will guide you through the process.
Step 6: Labor and Delivery with CPD

During labor and delivery with CPD, close monitoring and support are crucial. Here's what you can expect:
- Continuous Monitoring: Your healthcare team will closely monitor your vital signs, the baby's heart rate, and the progress of labor. This may involve the use of electronic fetal monitoring and regular vaginal examinations.
- Pain Management: Discuss pain management options with your healthcare provider. This may include epidural anesthesia or other methods to ensure your comfort during labor.
- Positioning and Support: Your healthcare team may guide you through different positions during labor to help facilitate the baby's descent through the birth canal. They may also provide physical support and encouragement throughout the process.
- Decision-Making During Labor: If complications arise or labor progresses slowly, your healthcare team will work with you to make informed decisions about the next steps. This may include the use of instruments like forceps or a vacuum extractor or the decision to proceed with a C-section.
Remember, the goal is to prioritize the safety and well-being of both you and your baby, and your healthcare team will provide the necessary support and guidance.
Step 7: Postpartum Care and Recovery

After delivery, whether by vaginal or cesarean birth, postpartum care and recovery are essential. Here's what you can expect:
- Postpartum Check-Ups: Attend all scheduled postpartum check-ups to monitor your recovery and the baby's well-being. These appointments are crucial for addressing any concerns and ensuring a smooth transition into motherhood.
- Pain Management: If you underwent a C-section, proper pain management is essential for a comfortable recovery. Follow your healthcare provider's instructions for pain medication and wound care.
- Breastfeeding Support: Breastfeeding can be challenging after a CPD delivery, but with support and guidance, it is possible. Lactation consultants and breastfeeding support groups can provide valuable assistance.
- Emotional Support: The postpartum period can be emotionally challenging, especially after a complicated delivery. Seek support from loved ones, join support groups, or consider counseling to process your emotions and adjust to your new role as a mother.
Remember, postpartum care is an essential part of the journey, and it's okay to ask for help and support during this time.
Step 8: Managing CPD in Future Pregnancies

If you've experienced CPD in a previous pregnancy, managing it in future pregnancies becomes a priority. Here are some key considerations:
- Prenatal Care and Monitoring: Start prenatal care early and attend all scheduled appointments. Regular monitoring and ultrasound scans can help track the growth and position of the baby, allowing for early detection of CPD and the development of a management plan.
- Consideration of Future C-Sections: If you've had a C-section due to CPD in the past, discuss the possibility of future C-sections with your healthcare provider. In some cases, a planned C-section may be recommended to minimize the risk of complications.
- Lifestyle Modifications: Maintaining a healthy weight, eating a balanced diet, and staying active during pregnancy can support optimal fetal growth and potentially reduce the risk of CPD.
Working closely with your healthcare team and staying informed about your options is crucial for managing CPD in future pregnancies.
Step 9: Emotional Support and Coping with CPD

Dealing with CPD can be emotionally challenging for expectant mothers and their partners. Here are some strategies for coping and finding support:
- Open Communication: Talk openly with your healthcare provider about your concerns and emotions. They can provide valuable guidance and support throughout the journey.
- Seek Support Groups: Joining support groups, either in-person or online, can connect you with other women who have experienced CPD. Sharing experiences and emotions can be therapeutic and provide a sense of community.
- Self-Care: Prioritize self-care during pregnancy and postpartum. This may include practicing relaxation techniques, engaging in activities you enjoy, and seeking emotional support from loved ones or professional counselors.
- Positive Affirmations: Focus on the positive aspects of your pregnancy and the upcoming arrival of your baby. Remind yourself that you are strong and capable, and that your healthcare team is there to support you every step of the way.
Remember, you are not alone, and there is support available to help you navigate the emotional challenges of CPD.
Step 10: Research and Advances in CPD Management
The field of obstetrics is constantly evolving, and researchers are dedicated to improving the management of CPD. Here are some ongoing areas of research and development:
- Non-Invasive Diagnostic Techniques: Researchers are exploring new, non-invasive methods for diagnosing CPD, such as advanced ultrasound techniques and 3D imaging.
- Improved Delivery Techniques: Ongoing research aims to develop safer and more effective delivery techniques for CPD, including the use of innovative instruments and minimally invasive procedures.
- Genetic and Environmental Factors: Studies are investigating the genetic and environmental factors that contribute to CPD, with the goal of developing targeted interventions and preventative measures.
- Patient Education and Empowerment: Efforts are being made to empower expectant mothers with knowledge and resources to make informed decisions about their care and advocate for their needs during pregnancy and childbirth.
Stay informed about the latest advancements in CPD management by following reputable sources and discussing them with your healthcare provider.
Conclusion
Managing Cephalopelvic Disproportion (CPD) requires a comprehensive and personalized approach. By understanding the signs, causes, and management strategies outlined in this guide, expectant mothers and their healthcare teams can navigate the challenges of CPD with confidence and optimism. Remember, early detection, regular prenatal care, and open communication with your healthcare provider are key to a successful outcome. With the right support and guidance, you can embrace the journey of motherhood, even in the face of CPD.
Frequently Asked Questions
What is the primary cause of CPD?
+The primary cause of CPD is a mismatch between the size of the baby’s head and the mother’s pelvis, often due to a combination of maternal and fetal factors.
Can CPD be prevented?
+While CPD cannot always be prevented, maintaining a healthy weight, eating a balanced diet, and staying active during pregnancy can support optimal fetal growth and potentially reduce the risk.
Is a C-section always necessary with CPD?
+No, a C-section is not always necessary with CPD. In some cases, a vaginal delivery may be attempted with close monitoring and support from a skilled healthcare team.
How can I cope with the emotional challenges of CPD?
+Seeking support from loved ones, joining support groups, and practicing self-care can help you cope with the emotional challenges of CPD. Open communication with your healthcare provider is also essential.
What are the long-term effects of CPD on future pregnancies?
+The long-term effects of CPD on future pregnancies can vary. Early detection, regular prenatal care, and open communication with your healthcare provider can help manage CPD effectively in subsequent pregnancies.